Our Services
-

Transcription
Convert your audio to text.
-

Subtitles
Add captions to your videos.
Supported Languages
Below is the list of popular languages we support for transcription and subtitles.
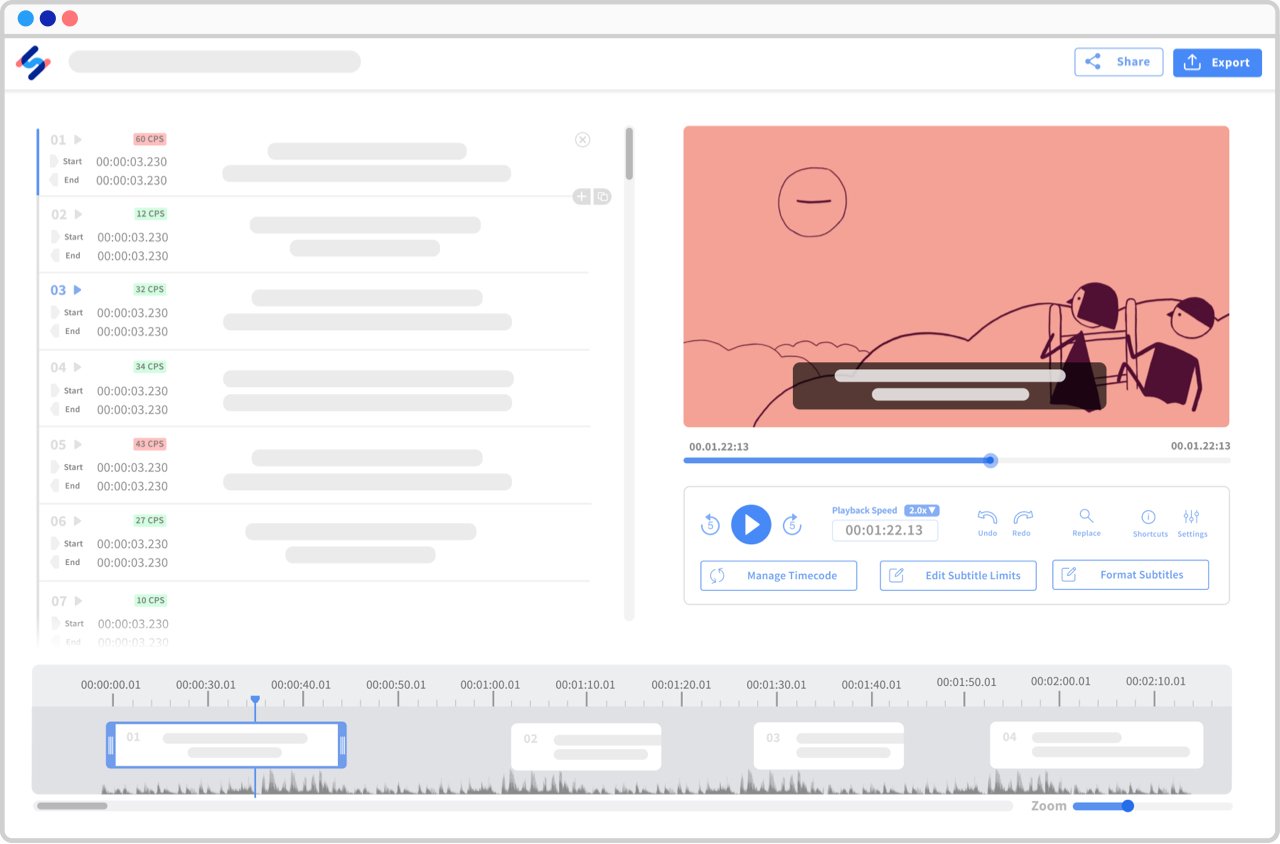
See all languages ▸Interactive editors, endless possibilities
Made for transcribers and subtitlers, our interactive editors will ease the way you interact with your transcripts and subtitles.
View a sample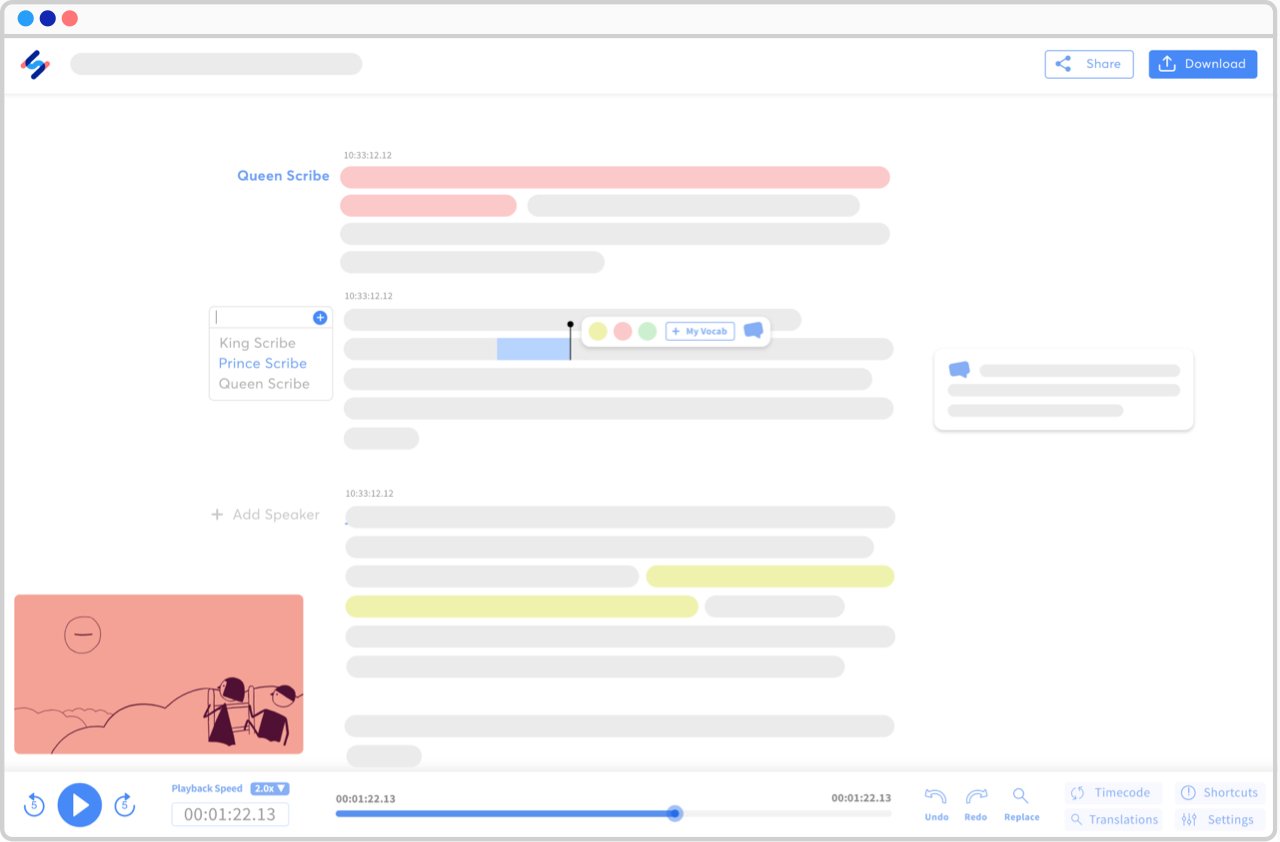
-

Sharing in a snap
Collaborate with all your stakeholders by sharing your transcripts and subtitles in view-only or edit mode — no matter where they are in the world.
-
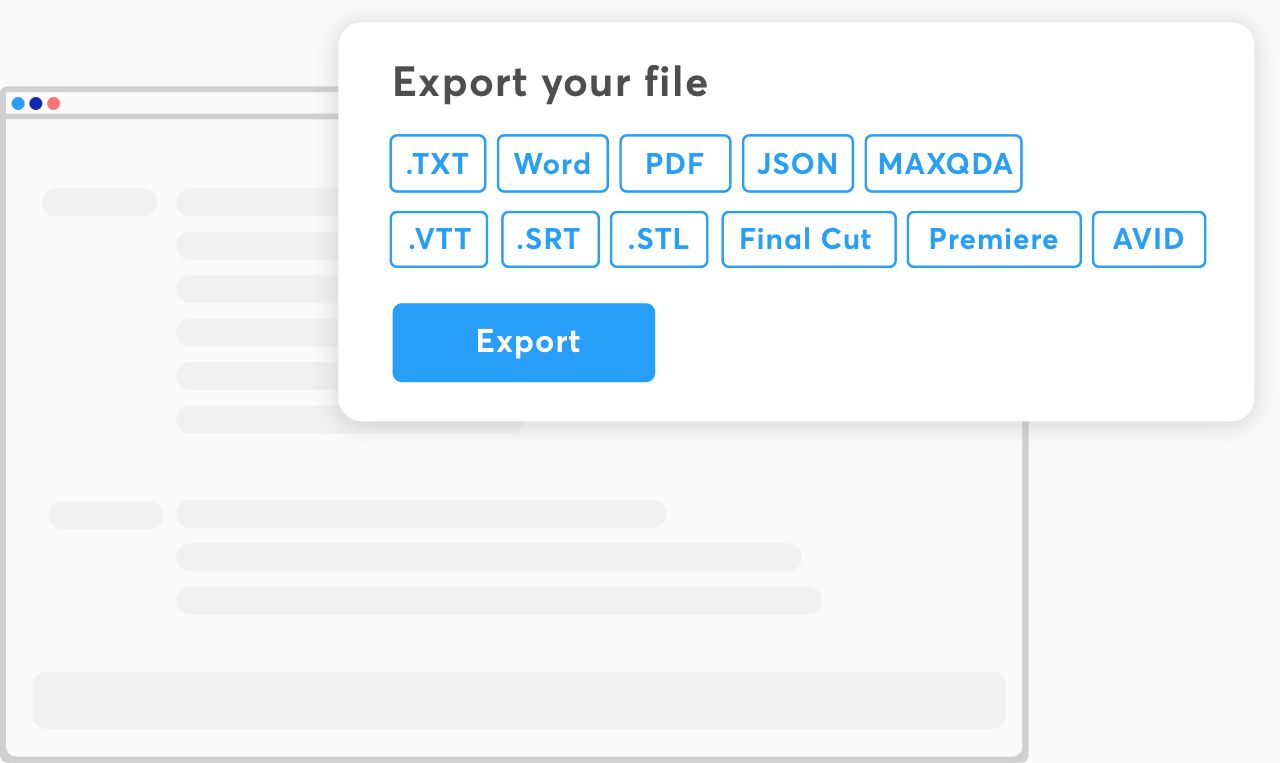
Multiple export formats
Export in all formats that you can think of. Our platform prepares you files that are ready for any kind of platform.
-
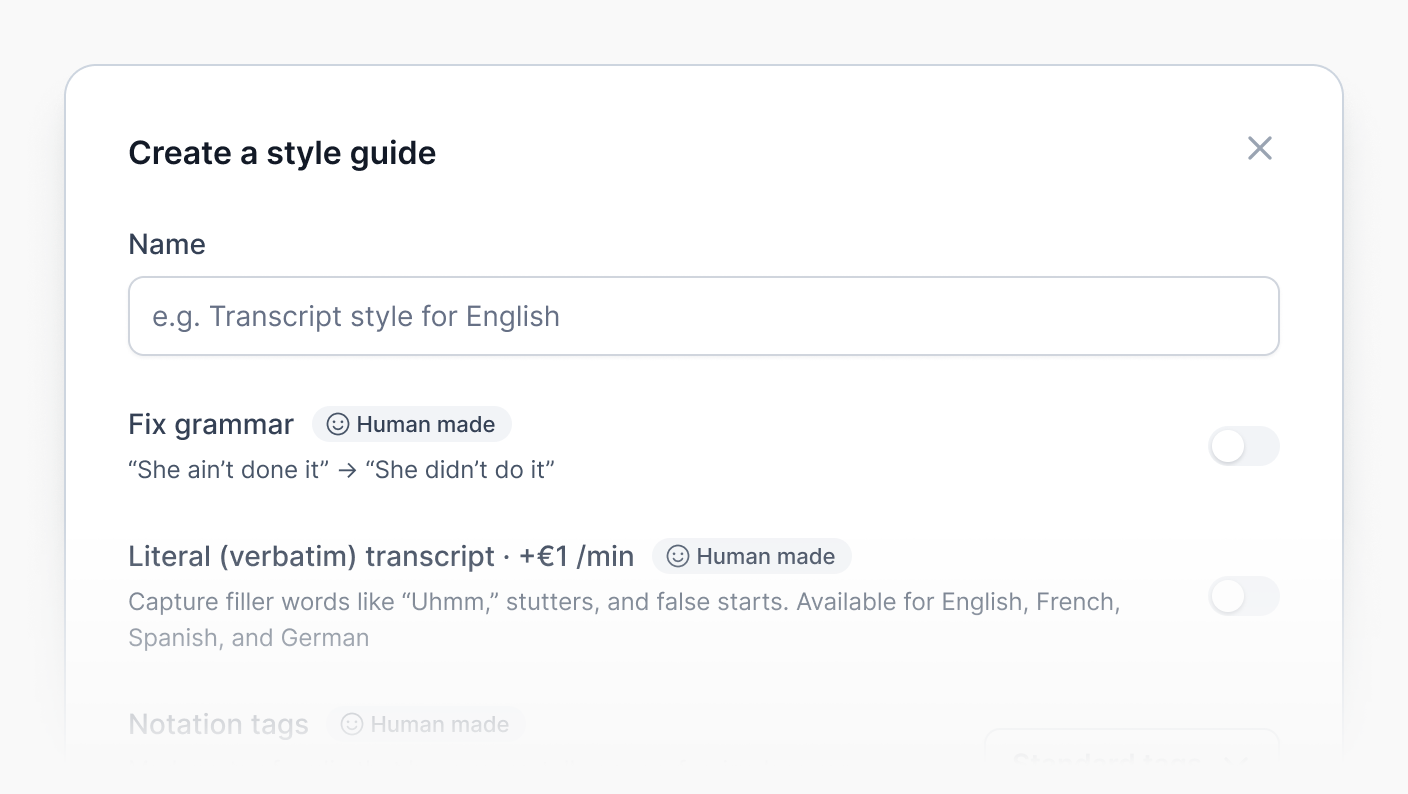
Netflix-quality subtitles with our style guide
Our style guide is tailored for project managers who demand precision, customization, and efficiency for their subtitling projects: choose your settings for timing, formatting, advanced grammar corrections, speaker identification, and more.
-
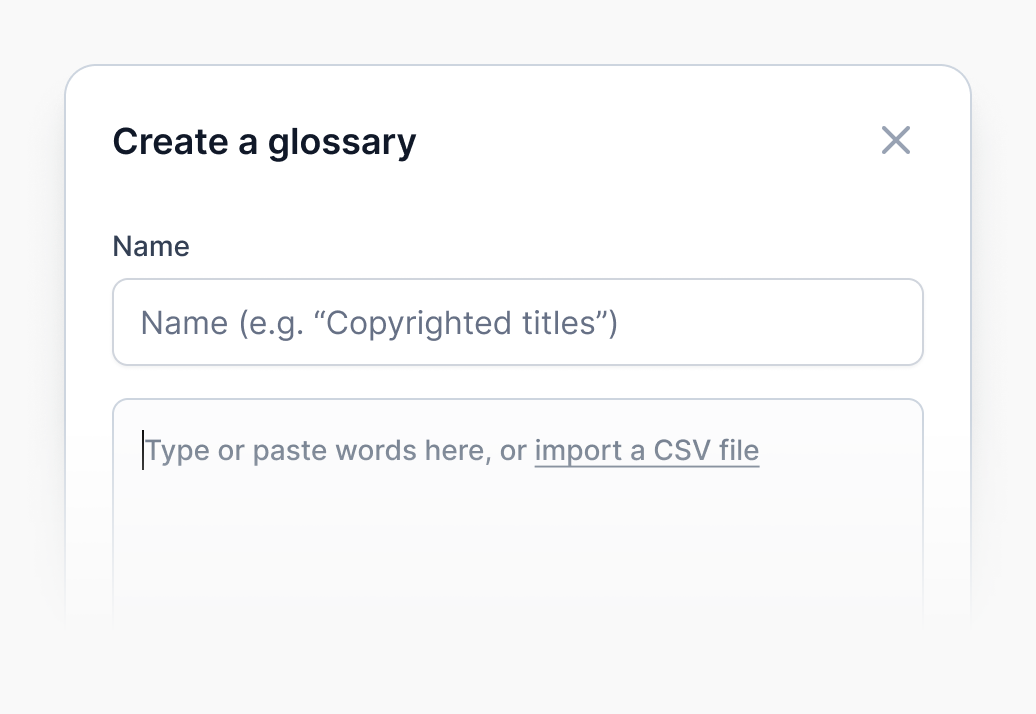
Glossaries and special guidelines
By adding specialized terminology (brands, slang, etc.) to a glossary, you can significantly reduce review time. We also support special guidelines, including SDH and verbatim, alongside a dedicated team of professional linguists.
Features
-
No limits on uploads
Upload files of any size and length. Our software supports them all.
-
Machine Translation
Automatically translate your transcription and subtitles in the most common languages.
-
Import from other platforms
Import any public links and synchronize Happy Scribe to your current workflow.
-
Workspaces for collaboration
Create spaces for you to share your files with the rest of your team.
-
APIs & Integrations
Seamlessly integrate with your favorite applications: Zapier, Youtube, and more.
-
Security & Confidentiality
All files are protected and remain private. Your subtitles are protected.
-
Best application on marketBest application on market. I love it !Sebastian Skowron - Trustpilot
-
It is a very good transcription…It is a very good transcription software. The incorporated text editor and the audio player allows to quickly follow and correct the automatic transcription. Highly recommended.Angel Efrén Guzmán V. - Trustpilot
-
Not badAlthough the transcription is not perfect by any means, the format makes it easier to transcribe.Qui Gon Gene - Trustpilot
-
Easy to use serviceEasy to use this service and I got exactly what I needed. I would definitely recommend to anyone who is looking for good, professional transcription services.Lynn Hayne - Trustpilot